Case Series/Study
(CS-054) The Use of a Transparent Gel Dressing in the Treatment of Deep-Tissue Pressure Injuries in an Acute Care Setting
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
Introduction: There is limited guidance regarding the use of dressings in the treatment of deep-tissue pressure injuries (DTPIs). Additionally, the repetitive removal of adhesive foam dressings can increase the risk of medical adhesive-related skin injury (MARSI). Transparent dressings can help protect the wounds from external contaminants and prevent further skin damage, while the clear design allows caregivers to quickly assess the skin without removing the dressing. One available transparent dressing is a transparent gel dressing (TGD) that is intended to be used as part of PI protocols. The dressing is designed with a transparent island to redistribute pressure and manage the microclimate of the wound.
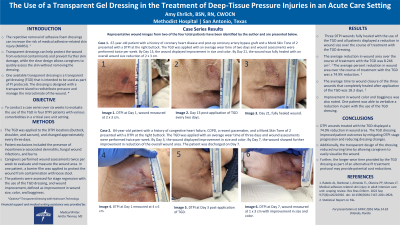
Methods: A case series was conducted over six weeks to evaluate the use of the TGD in four DTPI patients with various comorbidities in a critical care unit setting. The TGD was applied to the DTPI locations (buttocks, shoulder and sacrum), and changed every three days. Patient exclusions included the presence of incontinence-associated dermatitis, fungal wound infections and burns. Caregivers performed wound assessments twice per week to evaluate and measure the wounds. In one patient, a barrier film was applied to protect the wound from contamination with loose stool. The patients were assessed for stage regression with the use of the TGD dressing, and wound improvement, defined as improvement in wound size, color and bogginess.
Results: Each DTPI displayed a reduction in wound size (range of 3cm x 3cm to 0.2cm x 0.2cm reduction) over the course of treatment with the TGD dressing. Improvement in wound color and bogginess was also noted. Additionally, one patient was able to verbalize a reduction in pain with the use of the TGD dressing.
Discussion: The TGD dressing improved patient outcomes by mitigating DTPI stage progression and reducing dressing changes. Additionally, the transparent design of the dressing reduced nursing time by allowing caregivers to easily visualize the wound. Further, the longer wear time provided by the TGD as part of an alternative PI treatment protocol may provide potential cost reductions.
Methods: A case series was conducted over six weeks to evaluate the use of the TGD in four DTPI patients with various comorbidities in a critical care unit setting. The TGD was applied to the DTPI locations (buttocks, shoulder and sacrum), and changed every three days. Patient exclusions included the presence of incontinence-associated dermatitis, fungal wound infections and burns. Caregivers performed wound assessments twice per week to evaluate and measure the wounds. In one patient, a barrier film was applied to protect the wound from contamination with loose stool. The patients were assessed for stage regression with the use of the TGD dressing, and wound improvement, defined as improvement in wound size, color and bogginess.
Results: Each DTPI displayed a reduction in wound size (range of 3cm x 3cm to 0.2cm x 0.2cm reduction) over the course of treatment with the TGD dressing. Improvement in wound color and bogginess was also noted. Additionally, one patient was able to verbalize a reduction in pain with the use of the TGD dressing.
Discussion: The TGD dressing improved patient outcomes by mitigating DTPI stage progression and reducing dressing changes. Additionally, the transparent design of the dressing reduced nursing time by allowing caregivers to easily visualize the wound. Further, the longer wear time provided by the TGD as part of an alternative PI treatment protocol may provide potential cost reductions.

.jpeg)