Clinical Research
(CR-046) Clinical, Operational and Economic Benefits Associated with Implementing a Digitally-enabled Wound Care Program in Home Health
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
Kathleen Corcoran, BSN, RN,CWOCN,CHRN – AVP Wound care and Research, CenterWell Home Health; Robert D. J. Fraser, RN – Vice President Clinical Innovation, Clinical Research and Validation, Swift Medical Inc.; Kyle Lavergne, PhD – Vice President of Clinical Programs, CenterWell Home Health; Angela Graham, RN; Andrew Rauch, BA; Daniel Gill, BA – Director of Clinical Analytics & Financial Reporting; Shivika Singal, RN – AVP Clinical Systems & Innovation, CenterWell Home Health; Kwame Jones, BA – Senior Manager | Clinical Analytics; David Mannion, BA; Amy Cassata, BSN, RN, WCC – Senior Vice President Clinical Success, Clinical Success, Swift Medical Inc.
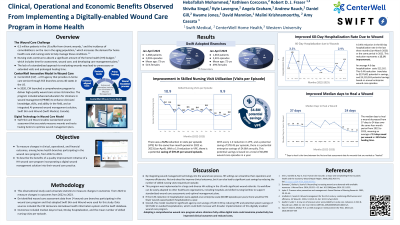
Introduction: A significant portion of the cost of home health (HH) is spent on nursing visits to assess and care for wounds.2 Hospitalization risk in a home health setting is increased by 52% when a patient requires wound care.1 To address this issue, one of the largest HH organizations operating across 40 states in the US has introduced a comprehensive wound care model (CWCM) with an integrated artificial intelligence-powered digital wound care solution (DWCS) to aid wound care delivery across 14 branches. This benefits evaluation study assessed the clinical, operational, and economic benefits of integrating the DWCS in HH.
Methods: The study compared outcomes from 2,003 wounds for the same four months (Jan-April) at 14 HH sites after adopting the CWCM in 2022 and from 2,401 episodes a year later. The data was collected from the site's electronic medical records and the DWCS databases, focusing on hospitalization rates at 30 and 60 days due to wounds, average days to heal wounds, and volume of visits per episode (VPE).
Results: Integrating DWCS showed promising results in reducing the hospitalization rate among wound patients in 2023 compared to the same period in 2022. There was a 0.8% reduction in the 30-day hospitalization rate, representing a 24% improvement, and a 0.4% reduction in the 60-day hospitalization rate, representing a 12% improvement. Additionally, all wound types experienced a significant reduction in 2023 vs. 2022 in days to heal, with an average of 13 days saved per wound or a 35% faster healing. Moreover, the adopted branches saw a significant 9.2% reduction in VPE. This process resulted in significant agency cost savings of $157,135 by reducing home care visits and up to $25,696,062 annual savings from avoided hospitalizations.
Discussion: Based on our results, integrating DWCS is critical to a high-performing wound care model in HH and implementing a CWCM. This model supports decision-making and improves organizations' capabilities while mitigating costs.
Methods: The study compared outcomes from 2,003 wounds for the same four months (Jan-April) at 14 HH sites after adopting the CWCM in 2022 and from 2,401 episodes a year later. The data was collected from the site's electronic medical records and the DWCS databases, focusing on hospitalization rates at 30 and 60 days due to wounds, average days to heal wounds, and volume of visits per episode (VPE).
Results: Integrating DWCS showed promising results in reducing the hospitalization rate among wound patients in 2023 compared to the same period in 2022. There was a 0.8% reduction in the 30-day hospitalization rate, representing a 24% improvement, and a 0.4% reduction in the 60-day hospitalization rate, representing a 12% improvement. Additionally, all wound types experienced a significant reduction in 2023 vs. 2022 in days to heal, with an average of 13 days saved per wound or a 35% faster healing. Moreover, the adopted branches saw a significant 9.2% reduction in VPE. This process resulted in significant agency cost savings of $157,135 by reducing home care visits and up to $25,696,062 annual savings from avoided hospitalizations.
Discussion: Based on our results, integrating DWCS is critical to a high-performing wound care model in HH and implementing a CWCM. This model supports decision-making and improves organizations' capabilities while mitigating costs.

.jpeg)