Clinical Research
(CR-025) Correlating Deep Vein Thrombosis in Femoral and Below Segments to Venous Leg Ulcer Incidence: Insights from a Retrospective Analysis
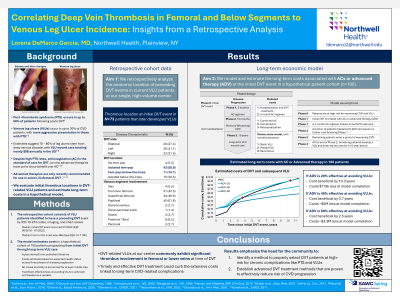
Venous leg ulcers (VLUs) represent the most advanced stage of chronic venous disease (CVD), often stemming from acute deep vein thrombosis (DVT). In the United States, VLUs affect a substantial population, annually impacting up to 600,000 patients and incurring approximately $3 billion in direct treatment costs alone [1]. However, these figures do not encompass indirect costs related to decreased quality of life, impaired work capacity, and disability. Addressing the initial occurrence of DVT may mitigate the socioeconomic burden associated with VLUs. In this work, we analyze the location of initial acute DVTs in VLU patients from a single high-volume center.
Methods:
Patients with VLUs were retrospectively identified by Current Procedural Terminology codes and included patients that experienced a first DVT event between August 2002 and July 2023. The locations of initial acute DVT were mapped from intravascular ultrasound and chart review.
Results:
In total, 73 patients were identified and included. Incident DVTs were iliofemoral-popliteal in 4/73 (5.5%), isolated femoral-popliteal in 43/73 (58.9%), femoral-popliteal with below-the-knee thrombus in 11/73 (15.1%), and isolated below-the-knee in 15/73 (20.5%). Therefore, femoral-popliteal thrombus was present in 58/73 (79.5%) and all patients (73/73) had thrombus present in the femoral veins or more distally.
Discussion:
Patients with VLUs at a high-volume CVD center commonly exhibit significant involvement in the femoral and below regions at their initial DVT diagnosis. Timely and effective intervention holds promise in curbing the extensive expenses linked to recurrent complications and long-term CVD-related complications. Consequently, these findings underscore the necessity for tailored tools aimed at addressing this overlooked patient cohort. Treatment guidelines [2], however, have been conservative towards treating isolated femoral DVT and below, which, coupled with a lack of extended follow-up and extensive tissue damage, compounds the existing challenges. Remaining questions persist regarding patient treatment strategies: is it imperative to address all individuals with femoral and below disease, or should our focus narrow to those presenting high-risk factors, like elevated body mass index, post-thrombotic incidents, and concurrent comorbidities such as smoking or diabetes?

.jpeg)