Clinical Research
(CR-039) The effect of Continuous Diffusion of Oxygen on breast tissue – Updated results from a Pilot Randomized Clinical Trial
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
Alejandro Zulbaran-Rojas, MD – Baylor College of Medicine; Rasha Bara, BS – Baylor College of Medicine; Miguel Bargas-Ochoa, MD – Baylor College of Medicine; Myeounggon Lee, PhD – Baylor College of Medicine; Sebastian Winocour, MD – Michael E. DeBakey Department of Surgery – Baylor College of Medicine; Alastair Thompson, MD – Michael E. DeBakey Department of Surgery – Baylor College of Medicine; Bijan Najafi, PhD, MSc – Baylor College of Medicine
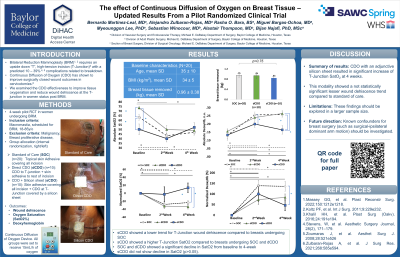
Introduction: Bilateral Reduction Mammoplasty (BRM)1, 2 requires the removal of breast tissue in women with macromastia. This procedure often requires an upside down “T”, high-tension incision (T-Junction)3 with known successful wound healing rates. However, cases with high tissue removal ( >750 gr) are susceptible to wound dehiscence at 1-month post-operative follow-up mostly due to low perfusion to the “T” junction4. Continuous Diffusion of Oxygen (CDO) has shown to improve surgically closed wound outcomes in patients undergoing lower neck surgery.5 This study examines the CDO effectiveness to improve tissue oxygenation and reduce wound dehiscence at the T-junction in women undergoing BRM.
Methods: A 4-week pilot randomized controlled trial in women undergoing BRM was conducted. The groups were internally randomized (left or right breast) to either receive standard of care (SOC) at the T-junction, SOC + CDO covered by a silicon sheet (sCDO), or CDO directly to the T-Junction skin (dCDO) for a 4-week duration. The primary outcome included T-junction wound dehiscence compared between the breast groups using Chi-square test. The secondary outcome included T-junction tissue saturation of oxygen (SatO2) assessed with Near-Infrared Spectroscopy (NIRS) and further analyzed with generalized linear model normalized to percentage change.
Results: Forty breasts (SOC, n=10; sCDO, n=10; dCDO, n=10) in twenty women (age= 35 ± 10 years, BMI= 34 ± 5 kg/m2) were included. The total breast tissue removal was 0.96±0.38 kg (p=0.75). At 4-week follow-up, breasts under sCDO showed a lower trend for T-Junction wound dehiscence compared to breasts undergoing SOC (0% vs 15%, p=0.19). In addition, breasts under sCDO showed a higher T-Junction SatO2 compared to breasts undergoing SOC (p=0.006, d=1.2) and dCDO (p< 0.001, d=1.6). Breasts under SOC and cDCO showed a significant decline in SatO2 from baseline to 4-week (p< 0.001, d=1.3; p< 0.001, d=2.7, respectively). However, breasts under sCDO did not show decline in SatO2 (p >0.05).
Discussion: CDO with an adjunctive silicon sheet resulted in significant increase of T-Junction SatO2 at 4 weeks. This modality showed a lesser wound dehiscence trend; however, it was not statistically significant. These findings should be explored in a higher sample size.
Methods: A 4-week pilot randomized controlled trial in women undergoing BRM was conducted. The groups were internally randomized (left or right breast) to either receive standard of care (SOC) at the T-junction, SOC + CDO covered by a silicon sheet (sCDO), or CDO directly to the T-Junction skin (dCDO) for a 4-week duration. The primary outcome included T-junction wound dehiscence compared between the breast groups using Chi-square test. The secondary outcome included T-junction tissue saturation of oxygen (SatO2) assessed with Near-Infrared Spectroscopy (NIRS) and further analyzed with generalized linear model normalized to percentage change.
Results: Forty breasts (SOC, n=10; sCDO, n=10; dCDO, n=10) in twenty women (age= 35 ± 10 years, BMI= 34 ± 5 kg/m2) were included. The total breast tissue removal was 0.96±0.38 kg (p=0.75). At 4-week follow-up, breasts under sCDO showed a lower trend for T-Junction wound dehiscence compared to breasts undergoing SOC (0% vs 15%, p=0.19). In addition, breasts under sCDO showed a higher T-Junction SatO2 compared to breasts undergoing SOC (p=0.006, d=1.2) and dCDO (p< 0.001, d=1.6). Breasts under SOC and cDCO showed a significant decline in SatO2 from baseline to 4-week (p< 0.001, d=1.3; p< 0.001, d=2.7, respectively). However, breasts under sCDO did not show decline in SatO2 (p >0.05).
Discussion: CDO with an adjunctive silicon sheet resulted in significant increase of T-Junction SatO2 at 4 weeks. This modality showed a lesser wound dehiscence trend; however, it was not statistically significant. These findings should be explored in a higher sample size.

.jpeg)