Clinical Research
(CR-008) Pressure Injury Reduction Through Increased Mobility and Pressure Redistribution
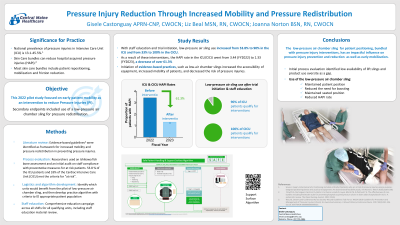
National prevalence of pressure injuries in ICU’s (Intensive Care Unit) is 13.1-45.5%. Skin Care bundles can reduce hospital acquired pressure injuries (HAPI) rates with a cost savings to the institution1 (Floyd, et al., 2021). Most skin care bundles include patient repositioning and mobilization as well as friction reduction.
Methods:
In 2022 a facility research group conducted an action study which included a literature review, protocol development, Ishikawa/fish bone assessment, staff education, and use of a low-pressure air chamber sling. This study followed the evidence-based guidelines of the Wound Ostomy Continence Nurses Society2 (WOCNS, 2016) to increase mobility and pressure redistribution in preventing pressure injuries. Researchers conducted an initial audit on staff compliance with preventative measures for patients identified at risk. 53.8 % of the ICU patients and 33% of the Cardiac Intensive Care Unit (CICU) met criteria for “at risk”. Initial process evaluation identified low availability of lift slings, as well as product oversite as a gap. In order to increase mobility of these critically ill patients, a trial of a low-pressure air chamber sling was initiated.
Results:
As a result of staff education and trial initiation low-pressure air sling use increased from 0-100% in the ICU and from 0-90% in the CICU. As a result of these interventions, the HAPI rate in the ICU/CICU went from 3.44 (FY2022) to 1.33 (FY2023). Initiation of evidenced-based practices such as low-air chamber slings increased the accessibility of equipment, increased mobility of patients and decreased the risk of pressure injuries.
Discussion: When an intervention is available that will redistribute pressure and increase mobility this may increase the RN use in ICU patients. Increasing any movement of ICU patients needs to be with the consideration of possible pressure injury

.jpeg)
