Case Series/Study
(LBA-003) A Case Report: Disseminated Cutaneous Coccidioidomycosis Mimicking Hidradenitis Suppurativa
Coccidioidomycosis, caused by dimorphic Coccidioides Immitis and Posadasii, rarely disseminates to skin but can present with challenging manifestation resembling various dermatological conditions. The disease is prevalent in arid regions and is acquired through inhalation of arthroconidia. This case report presents clinical features, diagnostic challenges, and management of disseminated cutaneous coccidioidomycosis (DCC) resembling hidradenitis suppurative (HS).
Methods:
A 31-year-old Hispanic male presented with worsening right inguinal and lower back (LB) pain secondary to abscess. He was in good health up until a year ago when he first developed right lateral thigh abscess, it self-drained and healed with scar. Six months later, he had another pustule draining lesion on right LB, s/p antibiotics, healed with scar. Three months ago, abscess formed at right inguinal and left LB which remained persistent despite multiple antibiotic regimens. Patient was seen in the ED 5-days prior to admission for new onset of symptoms: headache, subjective fever, nausea/vomiting, and left LB enlarging abscess, treated with I&D and antibiotics. His symptoms failed to resolve, and he returned to the hospital. Of note, patient reported severe cough 2-weeks prior to onset of first cutaneous lesion.
Results:
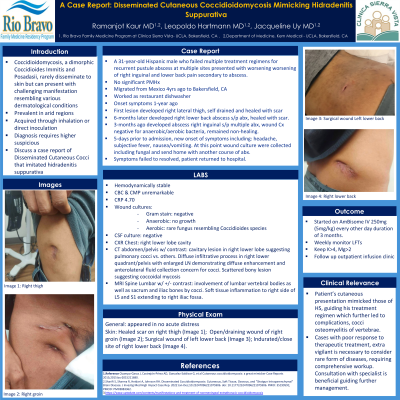
Patient was hemodynamically stable. Physical examination showed scar on right thigh (Image 1), open/draining wound of right inguinal site (Image 2), surgical wound of left LB (Image 3), indurated/closed site of right LB (Images 4).
Lab workup was unremarkable except wound culture showed rare fungus resembling coccidiosis’s species. Cocci serology reactive, CF titers 1:128. CXR showed right lower lobe cavitary lesion, confirmed with CT chest suggesting of pulmonary cocci. MRI lumbar showed involvement of vertebral bodies, sacrum, and iliac bones by coccidioidomycosis.
Discussion:
Patient’s cutaneous presentation mimicked those of HS, guiding his treatment regimen. Complications were due to failure to investigate broader differential diagnosis despite repeated treatment failure, resulting in DCC to the vertebral bodies. Cases with poor response to initial therapeutic treatment, extra vigilant is necessary to consider for rare form of diseases, requiring comprehensive workup including thorough culture studies, serological testing, and imaging. Consultation with specialist (e.g. Infectious Disease) is beneficial guiding further management. Patient was started on AmBisome IV 250mg (5mg/kg) every other day for duration of 3 months.

.jpeg)
