Clinical Research
(CR-038) Clinical evaluation of a novel, non-electrical single-use Negative Pressure Wound Therapy (NPWT) system for the management of closed surgical incisions
Thursday, May 16, 2024
2:15 PM - 3:15 PM East Coast USA Time
Jon Mathy, MD FACS FRACS – Plastic Surgeon, Regional Plastic Surgery Unit, Middlemore Clinical Trials and University of Auckland School of Medicine, New Zealand; Alpesh Patel, MBChB FRACS (Ortho) – Orthopaedic Surgeon, Middlemore Spinal Unit and Middlemore Clinical Trials, Auckland, New Zealand; John Buan, PhD – Chief Technical Officer, Aatru Medical, Cleveland, Ohio, USA; Jeffrey Ustin, MD MSc – Chief Medical Officer, Aatru Medical, LLC and UH Cleveland Medical Center, Cleveland, Ohio,USA.
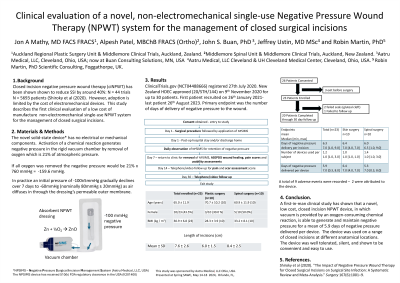
Introduction: Closed incision Negative Pressure Wound Therapy (ciNPWT) is a successful strategy to improve surgical outcomes. However, its use can be limited by the cost of electrically powered iNPWT systems, especially in developing countries. A novel NPWT* device that utilizes a chemical reaction to create negative pressure promises to be significantly less costly to manufacture.
Methods: A first-in-human clinical study was completed to evaluate the safety and performance of the novel iNPWT device. (NCT04488666). The primary endpoint was the longevity of the delivery of negative pressure to the wound over 7 days. Wound healing was assessed at day 7 and day 30. Scar quality at day 14 and day 30. Assessment of exudate management and ease of use were also undertaken.
Results: A total of 23 patients were enrolled in the study (mean age 65.0 ± 11.9; mean BMI 30.9 ± 6.8 (kg /m2) with a mean wound length of 7.6 ± 2.6 cm predominantly following elective plastic surgical and spinal surgery procedures. The new device maintained negative pressure and managed wound exudate for a mean of 6.06 ± 1.61 days per incision (n=16). The mean number of devices used per incision was 1.19 ± 0.54 (n=16). ASEPSIS and POSAS scores indicated overall normal wound healing and scar quality. There was a total of 9 Adverse Events in 5 patients. There were no Adverse Device Effects. Wounds treated with the new device were not painful. Participant and clinician assessments showed that the devices were easy to use and totally silent in operation. In spinal surgery patients, where increased shear forces place a greater strain on the dressing, 2 device failures prompted an enhanced design to improve adhesion of the port to the dressing.
Discussion:
A novel non-electrical iNPWT device has performed effectively in clinical use and shown to be convenient and easy to employ. Future studies should assess the effect on the level of surgical wound complications.
Methods: A first-in-human clinical study was completed to evaluate the safety and performance of the novel iNPWT device. (NCT04488666). The primary endpoint was the longevity of the delivery of negative pressure to the wound over 7 days. Wound healing was assessed at day 7 and day 30. Scar quality at day 14 and day 30. Assessment of exudate management and ease of use were also undertaken.
Results: A total of 23 patients were enrolled in the study (mean age 65.0 ± 11.9; mean BMI 30.9 ± 6.8 (kg /m2) with a mean wound length of 7.6 ± 2.6 cm predominantly following elective plastic surgical and spinal surgery procedures. The new device maintained negative pressure and managed wound exudate for a mean of 6.06 ± 1.61 days per incision (n=16). The mean number of devices used per incision was 1.19 ± 0.54 (n=16). ASEPSIS and POSAS scores indicated overall normal wound healing and scar quality. There was a total of 9 Adverse Events in 5 patients. There were no Adverse Device Effects. Wounds treated with the new device were not painful. Participant and clinician assessments showed that the devices were easy to use and totally silent in operation. In spinal surgery patients, where increased shear forces place a greater strain on the dressing, 2 device failures prompted an enhanced design to improve adhesion of the port to the dressing.
Discussion:
A novel non-electrical iNPWT device has performed effectively in clinical use and shown to be convenient and easy to employ. Future studies should assess the effect on the level of surgical wound complications.

.jpeg)
