Case Series/Study
(CS-115) Application of abductor digiti minimi muscle flap and synthetic electrospun fiber matrix after resection of osteomyelitis of fifth metatarsal: case series.
Osteomyelitis is a common complication associated with the diabetic foot.1 Surgical treatment of osteomyelitis involves debridement/ amputation of the involved tissue and bone.1 This can leave patients with large wound defects. Diabetic patients often experience poor wound healing related to poor circulation.2 Following surgical intervention, use of muscle flap may be considered to fill in the wound defect, cover exposed bones, improve local blood flow to the area and encourage healing.3,4
A synthetic electrospun fiber matrix (SEFM) could be considered to augment the flap procedures and reduce risk of necrosis. The engineered design of the electrospun matrix encourages cellular infiltration and neo-vascularization which could further support wound healing following flap procedures in a high-risk setting.5
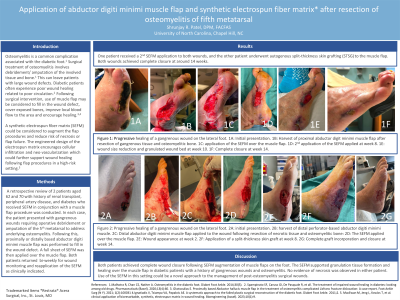
Methods: A retrospective review of 2 patients aged 62 and 70 with history of renal transplant, PAD, diabetes who received SEFM in conjunction with a muscle flap procedure was conducted. In each case, the patient presented with gangrenous wounds requiring operative debridement or amputation of the 5th metatarsal to address underlying osteomyelitis. Following this, proximally or distally based abductor digiti minimi muscle flap was performed to fill in the wound defect. A full sheet of SEFM was then applied over the muscle flap. Both patients returned to bi-weekly for wound monitoring and reapplication of the SEFM as clinically indicated.
Results:
One patient received a 2nd SEFM application to both wounds, and the other patient underwent autogenous split-thickness skin grafting (STSG) to the muscle flap. Both wounds achieved complete closure at 14 and 16 weeks.
Discussion:
Both patients achieved complete wound closure following SEFM augmentation of muscle flaps on the foot. The SEFM supported granulation tissue formation and healing over the muscle flap in diabetic patients with a history of gangrenous wounds and osteomyelitis. No evidence of necrosis was observed in either patient. Use of the SEFM in this setting could be a novel approach to the management of post-osteomyelitis surgical wounds.

.jpeg)