Clinical Research
(CR-054) Comparative Effectiveness of a Bilayered Living Cellular Construct and a Cryopreserved Cadaveric Skin Allograft for use in Pressure Injuries
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
Oscar Alvarez, PhD, CCT, FAPWCA – Adjunct Professor, Department of Surgery, Division of Plastic Surgery, Rutgers New Jersey Medical School
Introduction: Using real-world data (RWD) we conducted a comparative effectiveness analysis of Bilayered Living Cellular
Construct (BLCC)(a) versus Cryopreserved Cadaveric Skin Allograft (CCSA)(b) for the treatment of Pressure Injuries (PRIs).
Methods: Electronic medical records (WoundExpert®, Net Health, PA)(c) collected between 2020 and 2022, on 969 PRIs were analyzed. Ulcers 1-20 cm2 were included. Patients with no baseline wound measurements or follow-up visits were excluded. Evaluations were performed on 735 BLCC- and 234 CCSA- treated PRIs. A Cox analysis that adjusted for variables including ulcer area and duration was used to compute frequency and time to healing. The Hazard Ratio (HR) was computed to determine the probability of achieving healing throughout the study.
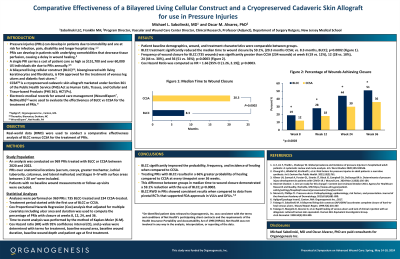
Results: Patient populations were well matched for patient demographics, wound characteristics, and treatment characteristics. The median time to healing was 20.3 months for CCSA and 8.3 months for BLCC; p=0.0002. This difference between groups demonstrated a 59.1% reduction in time to healing with the use of BLCC; p=0.0002. The frequency of healing for BLCC was significantly greater compared to CCSA at week 8 (19% vs 12%), 12 (28% vs 18%), 24 (44% vs 30%), and 36 (51% vs 36%); p=0.0003. The HR = 1.66 [95% CI (1.26, 2.19)]; p=0.0003. Treating PRIs with BLCC resulted in a 66% greater probability of healing compared to CCSA at every timepoint over 36 weeks.
Discussion: RWD analyses demonstrated that BLCC significantly improved healing compared to CCSA for the treatment of PRIs. These data may help guide decision-making in care of patients with PRIs. BLCC RWD in PRIs showed consistent results when compared to data from pivotal RCTs that supported FDA approvals in VLUs and DFUs.1,2
Construct (BLCC)(a) versus Cryopreserved Cadaveric Skin Allograft (CCSA)(b) for the treatment of Pressure Injuries (PRIs).
Methods: Electronic medical records (WoundExpert®, Net Health, PA)(c) collected between 2020 and 2022, on 969 PRIs were analyzed. Ulcers 1-20 cm2 were included. Patients with no baseline wound measurements or follow-up visits were excluded. Evaluations were performed on 735 BLCC- and 234 CCSA- treated PRIs. A Cox analysis that adjusted for variables including ulcer area and duration was used to compute frequency and time to healing. The Hazard Ratio (HR) was computed to determine the probability of achieving healing throughout the study.
Results: Patient populations were well matched for patient demographics, wound characteristics, and treatment characteristics. The median time to healing was 20.3 months for CCSA and 8.3 months for BLCC; p=0.0002. This difference between groups demonstrated a 59.1% reduction in time to healing with the use of BLCC; p=0.0002. The frequency of healing for BLCC was significantly greater compared to CCSA at week 8 (19% vs 12%), 12 (28% vs 18%), 24 (44% vs 30%), and 36 (51% vs 36%); p=0.0003. The HR = 1.66 [95% CI (1.26, 2.19)]; p=0.0003. Treating PRIs with BLCC resulted in a 66% greater probability of healing compared to CCSA at every timepoint over 36 weeks.
Discussion: RWD analyses demonstrated that BLCC significantly improved healing compared to CCSA for the treatment of PRIs. These data may help guide decision-making in care of patients with PRIs. BLCC RWD in PRIs showed consistent results when compared to data from pivotal RCTs that supported FDA approvals in VLUs and DFUs.1,2

.jpeg)