Case Series/Study
(CS-099) Delayed Application of Negative Pressure Wound Therapy Promotes Healing in Dehisced Surgical Wounds
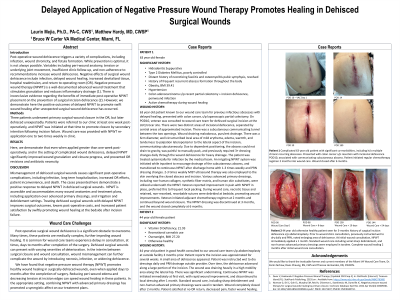
Post-operative wound dehiscence triggers a variety of complications, including infection, wound chronicity, and fistula formation. While prevention is optimal, it is not always possible. Variables including peri-wound anatomy, tension or underlying joint movement, insufficient clinic follow-up, and non-adherence to recommendations increase wound dehiscence. Negative effects of surgical wound dehiscence include infection, delayed wound healing, increased devitalized tissue, hospital readmission, and return to operating room (OR). Negative pressure wound therapy (NPWT) is a well-documented advanced wound treatment that stimulates granulation and reduces inflammatory drainage (1). There is inconclusive evidence regarding the benefits of immediate post-operative NPWT placement on the prevention of surgical incision dehiscence (2). However, we demonstrate here the positive outcomes of delayed NPWT to promote swift wound healing after unexpected surgical wound dehiscence has occurred.
Methods:
Three patients underwent primary surgical wound closure in the OR, but later dehisced unexpectedly. Patients were referred to our clinic at least one week post-operatively, and NPWT was initiated at that time to promote closure by secondary intention following incision failure. Wound care was provided with NPWT re-application one to two times weekly in clinic.
Results:
Here, we demonstrate that even when applied greater than one week post-operatively, and in the setting of complicated wound dehiscence, delayed NPWT significantly improved wound granulation and closure progress, and prevented OR revisions and antibiotic necessity.
Discussion:
Mismanagement of dehisced surgical wounds causes significant post-operative complications, including infection, long term hospitalization, increased OR efforts, patient inconvenience, and death. The cases presented here demonstrate a positive response to delayed NPWT in dehisced surgical wounds. NPWT is accessible and accommodates many wound anatomies and treatment plans, including application over advanced primary dressings, and irrigation and debridement settings. Treating dehisced surgical wounds with delayed NPWT improves surgical outcomes, lowers post-operative costs, and increased patient satisfaction by swiftly promoting wound healing at the bedside after incision failure.

.jpeg)