Case Series/Study
(CS-101) Don’t forget the VEIN, when treating venous stasis ulcerations
2.5 million Americans are diagnosed with chronic venous insufficiency, with over 20% later developing venous leg ulcers (VLUs). Over 30% of VLUs fail to heal in a 24-week period, despite multiple treatment options and algorithms. Recurrence rates can be as high as 70%, resulting in over $500 million in annual treatment cost of VLUs.[5] With chronic VLUs often taking months to years to heal, it is important not to forget to treat the underlying cause: the “vein” when attempting to heal these difficult wounds.
Methods:
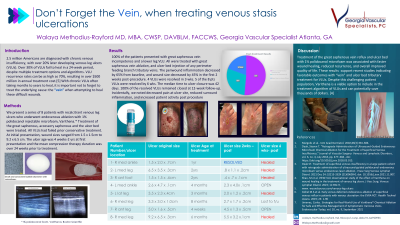
We present a series of 8 patients with recalcitrant venous leg ulcers who underwent endovenous ablation with 1% polidocanol injectable microfoam, Varithena. * Treatment of the great saphenous, accessory saphenous and the ulcer bed were treated. All VLUs had failed prior conservative treatment. At initial presentation, wound sizes ranged from 1.5 x 1.5cm to 9.2 x 6.5 cm. The ulcer age was 4 weeks-2 yrs at first presentation and the mean compression therapy duration was over 24 weeks prior to treatment.
Results:
100% of the patients presented with great saphenous vein incompetence and a lower leg VLU. All were treated with great saphenous vein ablation, and ulcer bed injection of any perimeter feeding branch tributary veins. The periwound inflammation decreased by 65% from baseline, and wound size decreased by 45% in the first 2 weeks post-procedure. 4 VLUs were resolved in 3 wks. 5 of the 8 pts VLUs were resolved by 6 wks. The median time to ulcer closure was 42 days. 100% of the resolved VLUs remained closed at 12-week follow-up. Incidentally, we noted decreased pain at ulcer site, reduced surround inflammation, and increased patient activity post procedure.
Discussion:
Treatment of the great saphenous vein reflux and ulcer bed with 1% polidocanol microfoam was associated with faster wound healing, reduced recurrence, and overall improved quality of life. These results support recent studies supporting the idea that treatment of the “vein” and ulcer bed tributaries when treating VLUs. Despite this challenging patient population, Varithena is a viable option to include in the treatment algorithm of VLUs and can potentially save thousands of dollars. [4]

.jpeg)