Clinical Research
(CR-051) Effectiveness of a novel polylactic acid matrix for diabetic foot ulcer closure: results from a single center interim analysis
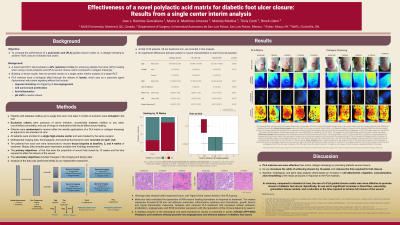
A recent pilot randomized clinical trial (RCT) demonstrated superiority for achieving diabetic foot ulcer (DFU) healing when using polylactic acid (PLA) closure matrices compared to the standard of care (SOC). Building on those results, here we present results on the interim analysis of a larger RCT using PLA matrices for DFU healing.
Methods:
Patients with diabetes and a single foot ulcer were randomized to receive weekly PLA matrices or collagen dressing applications. The wound size, time to attain full closure, and complications were recorded. Multispectral imaging data, thermography, and bacterial fluorescence were recorded on each visit. Ten patients from each arm were randomized to receive tissue biopsies at baseline, 2, and 4 weeks of treatment. Biopsy data includes gene expression analysis, bacterial load, and histology assessment. While this data is part of a multi-center RCT, for this interim analysis, all data comes from patients enrolled in a single high-volume center treated by the same surgeon. Analysis of the data was performed blindly by independent researchers.
Results:
A total of 50 patients, 25 per treatment arm, are included in this analysis. No significant differences between demographic or clinical characteristics were found between patient groups at baseline. All patients were followed until wound closure was achieved. The median time for achieving full closure in the collagen group was 17 weeks, compared to 9 weeks in the PLA group (reduction of 61.5%, p< 0.001). 32% vs 84% of wounds healed by 12 weeks in the collagen and PLA groups, respectively (p< 0.001). Multispectral data showed significantly higher oxygen content and higher temperatures in the PLA group. This was matched by more granulation tissue, increased collagen content, and more blood vessels in this group in the histology sections. Molecular data evaluated the expression of RNA wound healing biomarkers in response to treatment. The marker categories included ECM and cell adhesion molecules, inflammatory cytokines and chemokines, growth factors, and signal transduction molecules. Subjects who received PLA treatment had increased cellular adhesion, proliferation, angiogenesis, and ECM biomarker expression with the restoration of the immune balance by week 4. Quantification of bacterial load through the 16S rRNA gene demonstrated a significant reduction in the number of bacteria after 4 weeks of treatment.
Discussion:
These findings strongly suggest PLA matrices accelerate and facilitate wound healing. The mechanism of action of these matrices includes enhancement of cell attachment, proliferation, activity, vascularization, and pH shifts that inhibit bacterial overgrowth.

.jpeg)