Case Series/Study
(CS-079) Efficiency of New Smart Instillation Technology with Negative Pressure Wound Therapy in Managing Complex Chronic and Surgical Wounds: Case Series
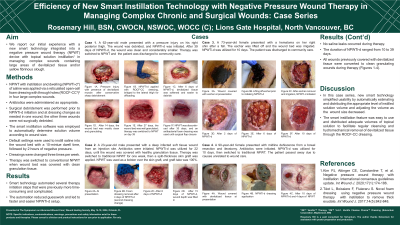
Use of negative pressure wound therapy with instillation and dwelling (NPWTi-d) of a topical wound solution has been limited in some settings due to perceptions of complexity of therapy set-up and support. NPWTi-d has become an important adjunct in our Level III trauma center to help manage complex wounds containing large areas of devitalized tissue and/or yellow fibrinous slough. We report our experience with a new smart instillation NPWTi-d system technology to reduce therapy setup complexity.
Methods:
NPWTi-d* with saline was applied via a reticulated open-cell foam dressing with through holes† (ROCF-CC) in three large complex wounds: a pressure injury, midline dehiscence from bowel resection and ileostomy, and a deep infected soft tissue wound from injection site. Antibiotics were administered as appropriate. Surgical debridement was performed initially on the pressure injury, and the other 2 wounds were not debrided. The smart instillation software‡ was employed to automatically determine solution volume according to wound size and to instill every 2 hours with a 10-minute dwell time between cycles. Dressings were changed 3 times/week. Therapy was switched to conventional NPWT when wound bed was covered with clean granulation tissue.
Results:
The smart technology automated several therapy initiation steps that previously were more time-consuming. Automation reduced guesswork and led to faster and easier NPWTi-d setup. Average duration of NPWTi-d was 17.7 days. All wounds previously covered with devitalized tissue were converted to clean granulating wounds during therapy. No saline leaks occurred during therapy.
Discussion:
In this patient series, new smart technology simplified usability by automatically estimating and distributing the appropriate level of instilled solution volume and adjusting the volume as the wound size decreased. The smart instillation feature was easy to use and distributed adequate volumes of topical solution to facilitate regular cleansing and removal of devitalized tissue through the ROCF-CC dressing.

.jpeg)
