Case Series/Study
(CS-033) Enzymatic Debriding Agent Eliminated and Accompanied by Other Improved Outcome Parameters
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
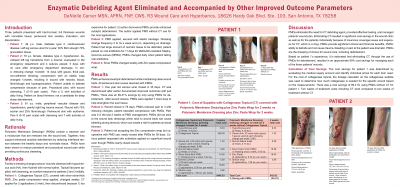
Introduction: Three patients presented with hard to heal wounds. Patient 1: 49 y.o. male, venous ulcer for a year. Prior wound care: soap/ water, topical creams, adhesive bandage. Patient 2: 79 y.o. female developed left leg hematoma from a trauma. The hematoma evacuated in the emergency department. 4 sutures were placed. The painful leg wrapped with gauze, elastic wrap for 19 days. Patient 3: 81 y.o. male, painful right leg trauma. Wound managed with soap/water, adhesive bandage for 35 days. All patients’ wounds had nonviable tissue; periwound skin swollen, induration, discoloration.
Methods: Patient 1: Collagenase Topical (CT), silver extra-thick Polymeric Membrane Dressing* (PMD), Zinc paste compression wrap applied, changed weekly. Wound management with CT for 2 applications, then discontinued as author found PMD worked well for autolytic debridement without CT. Patient 2: Managed 5 days post injury. Prior care before PMDs for 14 days: cleansed with Hypochlorous acid (HA), gauze, thick pad, non-adherent dressing, compression. PMD applied, elastic bandage. Dressing change frequency 2 to 3x a week and prn depending on drainage. Patient 3: Silver PMDs changed weekly with Zinc paste compression wrap. All patients’ wounds cleansed with each dressing change as per facility protocol; HA flushed with normal saline. Topical lidocaine applied with cleansing for patient 2 and 3.
Results: Patient 1: Wound closure 35 days. PMDs were applied 7 more days after closure to help strengthen the scar tissue. Patient 2: Wound closed 78 days. PMDs reduced pain. Patient 3: Uncooperative with Zinc compression wrap but cooperative with PMD use, almost at wound closure with PMDs 39 days. Skin substitute applied on superficial wound at patient request, wanted to try it even though PMDs almost closing wound. PMDs enhanced autolytic debridement while maintaining clean wound beds. All periwound skin issues were resolved with PMDs.
Discussion: PMDs provided effective healing, managed patients’ pain and eliminated the need for CT debriding agent. There was overall cost savings across clinic-patient copay, insurance coverage with using PMDs vs. CT. PMDs ability to debride and not cause increased trauma, bleeding or pain to the patient was dramatic.
Methods: Patient 1: Collagenase Topical (CT), silver extra-thick Polymeric Membrane Dressing* (PMD), Zinc paste compression wrap applied, changed weekly. Wound management with CT for 2 applications, then discontinued as author found PMD worked well for autolytic debridement without CT. Patient 2: Managed 5 days post injury. Prior care before PMDs for 14 days: cleansed with Hypochlorous acid (HA), gauze, thick pad, non-adherent dressing, compression. PMD applied, elastic bandage. Dressing change frequency 2 to 3x a week and prn depending on drainage. Patient 3: Silver PMDs changed weekly with Zinc paste compression wrap. All patients’ wounds cleansed with each dressing change as per facility protocol; HA flushed with normal saline. Topical lidocaine applied with cleansing for patient 2 and 3.
Results: Patient 1: Wound closure 35 days. PMDs were applied 7 more days after closure to help strengthen the scar tissue. Patient 2: Wound closed 78 days. PMDs reduced pain. Patient 3: Uncooperative with Zinc compression wrap but cooperative with PMD use, almost at wound closure with PMDs 39 days. Skin substitute applied on superficial wound at patient request, wanted to try it even though PMDs almost closing wound. PMDs enhanced autolytic debridement while maintaining clean wound beds. All periwound skin issues were resolved with PMDs.
Discussion: PMDs provided effective healing, managed patients’ pain and eliminated the need for CT debriding agent. There was overall cost savings across clinic-patient copay, insurance coverage with using PMDs vs. CT. PMDs ability to debride and not cause increased trauma, bleeding or pain to the patient was dramatic.

.jpeg)