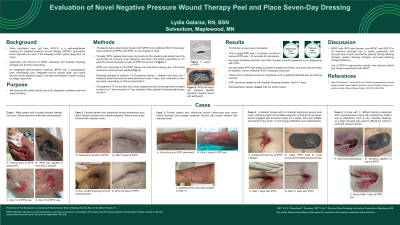
Case Series/Study
(CS-061) Evaluation of Novel Negative Pressure Wound Therapy Peel and Place Seven-Day Dressing
While reticulated open cell foam (ROCF) is a well-established dressing for negative pressure wound therapy (NPWT), granulation tissue ingrowth can occur if the dressing is left in place longer than 72 hours, potentially causing wound bed disruption, bleeding, and pain upon dressing removal. Additionally, sizing the foam to fit the wound can be time-consuming. A novel multilayer peel and place dressing (MPPD) with a polyurethane foam manifolding core and hybrid silicone-acrylic adhesive drape1 has been developed to remain in place for longer wear time. We report the results of a MPPD user evaluation study.
Methods:
Ten patients being adjunctively treated with NPWT with traditional ROCF dressings* were switched to NPWT with MPPD at one hospital in Chile. MPPD was applied in similar fashion by three clinicians: release liners were removed and dressing was placed on the wound bed as a wound cover dressing, with foam core portion extending ≥1 cm past the wound perimeter. MPPD was connected to the NPWT device via multi-lumen tubing, and -125 mmHg continuous pressure was applied. Dressing changes for patients 1-5 (3 pressure injuries, 1 diabetic foot ulcer, and 1 dehisced abdominal wound) were performed every 3 days, then switched to once per week, depending on clinical presentation. Dressings were changed on days 5 or 7, then moved to a 7-day schedule for patients 6-10 (3 traumatic and 2 post-surgical wounds). Patient 6 discontinued therapy on day 5.
Results:
10 clinician surveys were completed. Time to apply MPPD was < 3 minutes, and time to remove MPPD was < 20 seconds for all patients. No patients reported pain at dressing removal, and no adverse events or complaints were reported. Surveys stated MPPD was easier and faster to apply and remove, and much less traumatic for patients, versus traditional ROCF dressings used prior. MPPD remained sealed for the intended dressing duration, from 4-7 days.
Discussion:
NPWT with MPPD was favored over NPWT with ROCF by all clinicians surveyed due to easier application and removal, lack of pain reported by patients during dressing changes, quicker dressing changes, and lower dressing change frequency. Use of MPPD in appropriate wounds may improve patient and clinician experience with NPWT.

.jpeg)
