Clinical Research
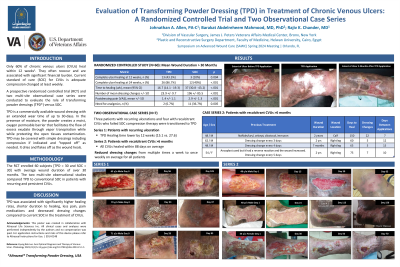
(CR-001 (RPT-004)) Evaluation of Transforming Powder Dressing (TPD) in Treatment of Chronic Venous Ulcers: A Randomized Controlled Trial and Two Observational Case Series
Only 60% of chronic venous ulcers (CVUs) heal within 12 weeks, often recur, and are associated with significant financial burden. Current standard of care (SOC) for CVUs is adequate compression changed at least weekly.
A prospective randomized controlled trial (RCT) and two multi-site observational case series were conducted to evaluate the role of transforming powder dressing (TPD) with compression in CVU management compared to SOC (compression). TPD transforms upon hydration into a shape-retentive matrix to create optimum moist wound healing conditions.
Methods:
The RCT enrolled 60 subjects [TPD = 30 and SOC = 30] with an average wound duration of over 30 months. The two multi-site observational studies compared TPD to conventional SOC in patients with persistent CVUs.
Results:
In the RCT, the TPD cohort had significantly higher rates of complete ulcer healing at 12 weeks (43.3% vs 10.0%, p = .004) and 24 weeks (86.7% vs 40.0%, p < .001) when compared with SOC. The TPD group had significantly shorter average time (weeks) to complete healing [16.7 versus 37.0, p < .001], significantly fewer dressing changes (23.9 vs 196.0, p < .001), less pain (VAS 1.4 vs 2.9, p < .001) and lower incidence of required pain medications (2% vs 11%, p = .005).
The first observational series evaluated 3 patients with recurring ulceration who initially underwent conventional SOC compression therapy. TPD was utilized on the recurring ulcers and patients served as their own control. Healing time was lower by 12 weeks (15.1 vs 27.6) while using TPD and dressing changes requirements were reduced from multiple times a week to once weekly.
The second observational series, evaluated 4 patients with recalcitrant CVUs treated unsuccessfully with SOC compression for >6 months. Upon conversion to TPD, all CVUs healed within 88 days on average. Dressing changes were reduced from multiple times per week to once weekly.
Discussion:
TPD was associated with significantly higher healing rates, shorter duration to healing, less pain, and decreased dressing changes compared to current SOC in the treatment of CVUs. Overall, use of TPD resulted in improved patient satisfaction and decreased financial burden.

.jpeg)
