Case Series/Study
(CS-076) Healing a large Moh’s surgical wound due to squamous cell skin cancer with Icelandic Cod Fish skin
There are approximately 1.8 million cases of squamous cell skin cancer diagnosed in the United States annually. Many patients and dermatologists opt for Mohs Microdermagraphic surgery to treat these lesions. However, the wounds can become quite large and deep depending on how large the lesion is as well as the depth. It is not uncommon to have exposed bone in the base of some of these wounds.
Methods:
A 68 yo female with a history of end stage renal disease due to Systemic Lupus Erythematosis, HTN, Chronic Venous Insufficiency (CVI),Ethanol abuse, and frequent falls presented to our Wound Clinic after undergoing Moh’s microdermagraphic surgery on 5/23/2023 for a large squamous cell skin cancer on the distal right anterior tibial area. Wound was full thickness and almost down to bone. Pt is not diabetic. She does not smoke. She consumes approximately 3 shots of alcohol per day. She is chronically immunosuppressed due to the her SLE. She had multiple reasons for not being able to heal this complex wound including her comorbidities, the location and extent of the wound, and her chronic steroid dependence.
Results:
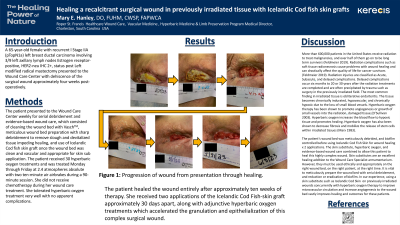
This is a case report of a large, full thickness Moh’s microdermagraphic surgical wound on a distal extremity in an immunosuppressed patient with end stage renal disease on hemodialysis. Wounds on the anterior tibial area are notoriously hard to heal due to their location and paucity of subcutaneous tissue and blood vessels. This patient had every reason to NOT heal this wound, but with meticulous wound care, serial debridement, appropriate use of culture directed antibiotic therapy as indicated, biofilm management and judicious use of Icelandic Cod fish skin on a well prepared wound, she was able to go on to complete healing.
Discussion: The patient’s wound required meticulous wound bed preparation and maintenance to minimize slough, eschar and biofilm. The patient required weekly to biweekly visits over several months and was compliant with all treatments. The patient’s insurance did not cover the cost of the Icelandic Cod Fish Skin substitute, so it was donated by the company out of a compassionate care program. She had such an excellent response to one treatment only, that further application was not deemed warranted.
The patient’s wound had stagnated, and a single application of Icelandic Cod Fish skin successfully reanimated the wound to progress toward complete healing.

.jpeg)