Clinical Research
(CR-032) Image-Guided Scalpel Debridement of Diabetic Foot Ulcers Using a Smartphone-based Tissue Oxygenation Tool
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
Kacie Kaile, PhD – Biomedical Engineering – Florida International University; Maria Hernandez, BS student – Biomedical Engineering – Florida International University; Renata Sousa, DPM – White Memorial Medical Group; Jose Ponce, DPM – White Memorial Medical Group; Stanley Mathis, DPM – Clemente Clinical Research; Alexander Trinidad, BS; Nikhil vedere, BS – Florida International University; Himaddri Roy, BS – Biomedical Engineering – Florida International University; Manuel Leizaola, BS student; David Armstrong, DPM, PhD – Keck School of Medicine – University of Southern California; Anuradha Godavarty, PhD – Biomedical Engineering – Florida International University
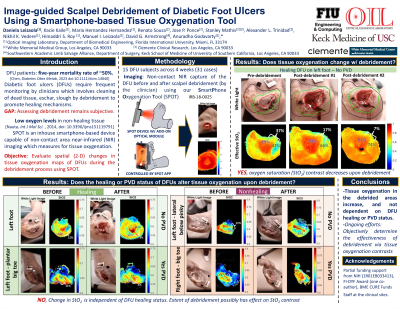
Introduction: Diabetic foot ulcers (DFUs) are one of the most common complications for diabetics [1,2]. Wound healing requires oxygen to reach the wound bed for cellular processes to occur. Our past studies have investigated tissue oxygenation to assess the wound healing status [3] and the DFUs that required clinical (surgical) intervention [4]. In most DFU cases, the typical outpatient intervention involves scalpel debridement to remove unviable tissue and promote healing. However, the effectiveness of how debridement improves oxygenated blood flow to the region is not objectively assessed. The goal of this study is to perform image-guided scalpel debridement of DFUs using a smartphone-based optical imaging device to determine the extent of tissue oxygenation changes in response to the procedure.
Methods: In this IRB approved study, DFU patients (n=15) were imaged with our in-house near-infrared optical imager (smartphone oxygenation tool, SPOT) before and after the scalpel debridement procedure. The optical images were processed to obtain tissue oxygenation based parameters (effective oxyhemoglobin, deoxyhemoglobin, oxygen saturation and total hemoglobin) of the wound area [5,6]. The tissue oxygenation parameters were compared between the wound and its immediate surroundings (peri-wound) before and after the debridement process. Contrast values were calculated as a ratio of tissue oxygenation parameter between the wound and periwound regions (demarcated by the clinicians).
Results: Qualitative comparisons showed the wound region had a higher oxygen saturation than the periwound prior to debridement. This difference in oxygen saturation between the wound and peri-wound regions distinctly reduced after the debridement process. Quantitatitative analysis pre- and post-debridement were compared by changes in the contrast values. A sample pre-debridement case showed the wound region to have a 37% higher oxygen saturation than that in the callused peri-wound regions. This contrast decreased to 7% difference post-debridement. Our ongoing work involves the quantification of the differences in the tissue oxygenation pre- and post-debridement across all DFU cases and across all their weeks of treatment (up to 4 weeks).
Discussion: Scalpel debridement removes non-viable tissue that impedes healing. Regions with low oxygen saturation correlated with regions that were debrided. Hence, non-viable tissue could be visible in tissue oxygenation maps and potentially indicate regions requiring debridement. SPOT’s tissue oxygenation maps obtained during the debridement process could serve as an objective image-guided tool to determine effective scalpel tissue removal.
Methods: In this IRB approved study, DFU patients (n=15) were imaged with our in-house near-infrared optical imager (smartphone oxygenation tool, SPOT) before and after the scalpel debridement procedure. The optical images were processed to obtain tissue oxygenation based parameters (effective oxyhemoglobin, deoxyhemoglobin, oxygen saturation and total hemoglobin) of the wound area [5,6]. The tissue oxygenation parameters were compared between the wound and its immediate surroundings (peri-wound) before and after the debridement process. Contrast values were calculated as a ratio of tissue oxygenation parameter between the wound and periwound regions (demarcated by the clinicians).
Results: Qualitative comparisons showed the wound region had a higher oxygen saturation than the periwound prior to debridement. This difference in oxygen saturation between the wound and peri-wound regions distinctly reduced after the debridement process. Quantitatitative analysis pre- and post-debridement were compared by changes in the contrast values. A sample pre-debridement case showed the wound region to have a 37% higher oxygen saturation than that in the callused peri-wound regions. This contrast decreased to 7% difference post-debridement. Our ongoing work involves the quantification of the differences in the tissue oxygenation pre- and post-debridement across all DFU cases and across all their weeks of treatment (up to 4 weeks).
Discussion: Scalpel debridement removes non-viable tissue that impedes healing. Regions with low oxygen saturation correlated with regions that were debrided. Hence, non-viable tissue could be visible in tissue oxygenation maps and potentially indicate regions requiring debridement. SPOT’s tissue oxygenation maps obtained during the debridement process could serve as an objective image-guided tool to determine effective scalpel tissue removal.

.jpeg)