Clinical Research
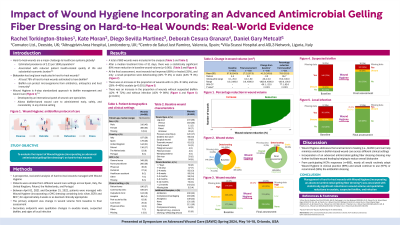
(CR-057) Impact of Wound Hygiene incorporating an advanced antimicrobial gelling fiber dressing on hard-to heal wounds: real-world evidence
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
Kate Moran, Tissue Viability Nurse – Altnagelvin Area Hospital; Diego Sevilla Martinez, Nurse – Centro de Salud Just Ramírez; Deborah Cesura Granara, Wound Care Nurse Specialist – Villa Scassi Hospital; Daniel Metcalf, PhD – Director, Advanced Wound Care R&D, Convatec
Introduction: Hard-to-heal wounds are an increasing challenge in wound care and are associated with surface-associated and aggregated communities of microorganisms embedded in a self-produced matrix of extracellular polymeric substances.1 The aim of this real-world study was to evaluate the impact of Wound Hygiene (WH), a 4-step (cleanse, debride, refashion, and dress) wound management protocol on hard-to-heal wounds.
Methods: A prospective, real-world analysis of hard-to-heal wounds managed with WH incorporating a carboxymethylcellulose dressing containing ionic silver, ethylenediaminetetraacetic acid, and benzethonium chloride,1 for approximately 4 weeks or as deemed clinically appropriate. The primary endpoint was change in wound volume from baseline to final assessment.
Results: 693 wounds were included in the analysis (median treatment duration 31 days). Most healthcare professionals were general nurses (50%) or advanced practitioners (38%). Patient homes (27%) and community clinics (27%) were the most common clinical settings. Venous leg ulcers were the most common wound type (26%) followed by pressure ulcers/injuries (17%); duration of wounds was >12 months in 21% of cases. The mean wound volume was 57.8 cm3 at baseline and was 17.2 cm3 at final assessment. There was an 80% reduction in wound volume from baseline to final assessment (p< 0.001; calculation excludes wounds with zero wound depth at baseline). At baseline, 66% of wounds were static or deteriorating; at final assessment, this had decreased to 5%, and 94% improved or healed. Exudate levels were moderate or high in 69% of cases at baseline which decreased to 25% at final assessment (p< 0.001). Local wound infection decreased from 43%, at baseline to 3% at final assessment (p< 0.001).
Discussion: Management with WH resulted in healing or improvement in nearly all hard-to heal wounds by final assessment, with a statistically significant decrease in wound volume, exudate level, and local infection.
Methods: A prospective, real-world analysis of hard-to-heal wounds managed with WH incorporating a carboxymethylcellulose dressing containing ionic silver, ethylenediaminetetraacetic acid, and benzethonium chloride,1 for approximately 4 weeks or as deemed clinically appropriate. The primary endpoint was change in wound volume from baseline to final assessment.
Results: 693 wounds were included in the analysis (median treatment duration 31 days). Most healthcare professionals were general nurses (50%) or advanced practitioners (38%). Patient homes (27%) and community clinics (27%) were the most common clinical settings. Venous leg ulcers were the most common wound type (26%) followed by pressure ulcers/injuries (17%); duration of wounds was >12 months in 21% of cases. The mean wound volume was 57.8 cm3 at baseline and was 17.2 cm3 at final assessment. There was an 80% reduction in wound volume from baseline to final assessment (p< 0.001; calculation excludes wounds with zero wound depth at baseline). At baseline, 66% of wounds were static or deteriorating; at final assessment, this had decreased to 5%, and 94% improved or healed. Exudate levels were moderate or high in 69% of cases at baseline which decreased to 25% at final assessment (p< 0.001). Local wound infection decreased from 43%, at baseline to 3% at final assessment (p< 0.001).
Discussion: Management with WH resulted in healing or improvement in nearly all hard-to heal wounds by final assessment, with a statistically significant decrease in wound volume, exudate level, and local infection.

.jpeg)