Clinical Research
(CR-058) Impact of Wound Hygiene incorporating an advanced antimicrobial gelling fiber dressing on hard-to-heal wounds treated with antibiotics
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
Daniel Metcalf, PhD – Director, Advanced Wound Care R&D, Convatec
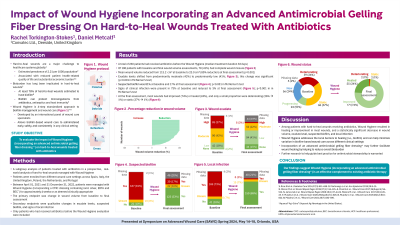
Introduction: Microbial bioburden has long been implicated as a barrier to healing in hard-to-heal wounds and is often comprised of surface-associated and aggregated communities of microorganisms that are embedded in a self-produced matrix of extracellular polymeric substances.1 We evaluated the impact of Wound Hygiene (WH), a 4-step (cleanse, debride, refashion, and dress) wound management strategy, on hard-to-heal wounds that were being treated with antibiotics.
Methods: A subgroup analysis of patients treated with antibiotics in a prospective, real-world study of hard-to-heal wounds managed with WH (incorporating an advanced antimicrobial gelling fiber dressing*) for approximately 4 weeks, or as clinically appropriate, was performed. The primary endpoint was change in wound volume from baseline to the final assessment. Only patients who had received antibiotics before the WH evaluation were included.
Results: 230 patients had received antibiotics before the WH evaluation (median WH treatment duration 33 days). Of 190 wounds with baseline and final wound volume assessments, 79 (42%) had complete wound closure (zero volume). Mean wound volume reduced from 112.9 cm3 at baseline to 23.0 cm3 (80% reduction) at final assessment (p< 0.001). Exudate levels changed from predominantly moderate (42%) to predominantly low (40%) (p< 0.001). Signs of clinical infection were present in 74% of wounds at baseline and reduced to 3% at final assessment (p< 0.001). At final assessment, 24% of wounds had healed and 74% had improved.
Discussion: Among patients with hard-to-heal wounds receiving antibiotics, WH resulted in closure or improvement in most wounds, and a statistically significant decrease in wound volume, exudate level, and local infection. Our findings suggest WH is an effective complement to existing antibiotic therapy. Further research to help guide best practice for antimicrobial stewardship is warranted.
Methods: A subgroup analysis of patients treated with antibiotics in a prospective, real-world study of hard-to-heal wounds managed with WH (incorporating an advanced antimicrobial gelling fiber dressing*) for approximately 4 weeks, or as clinically appropriate, was performed. The primary endpoint was change in wound volume from baseline to the final assessment. Only patients who had received antibiotics before the WH evaluation were included.
Results: 230 patients had received antibiotics before the WH evaluation (median WH treatment duration 33 days). Of 190 wounds with baseline and final wound volume assessments, 79 (42%) had complete wound closure (zero volume). Mean wound volume reduced from 112.9 cm3 at baseline to 23.0 cm3 (80% reduction) at final assessment (p< 0.001). Exudate levels changed from predominantly moderate (42%) to predominantly low (40%) (p< 0.001). Signs of clinical infection were present in 74% of wounds at baseline and reduced to 3% at final assessment (p< 0.001). At final assessment, 24% of wounds had healed and 74% had improved.
Discussion: Among patients with hard-to-heal wounds receiving antibiotics, WH resulted in closure or improvement in most wounds, and a statistically significant decrease in wound volume, exudate level, and local infection. Our findings suggest WH is an effective complement to existing antibiotic therapy. Further research to help guide best practice for antimicrobial stewardship is warranted.

.jpeg)