Clinical Research
(CR-052 (RPT-006)) Polylactic acid matrices directly promote neo-angiogenesis and immune balance in diabetic foot ulcers
Methods:
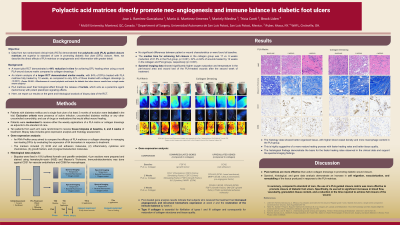
Patients with diabetes and a single foot ulcer were randomized to receive weekly PLA matrices or collagen dressing. The trial’s primary endpoints were the time to attain full closure and the rate of full healing by 12 weeks. Near-infrared multispectral imaging and infrared thermography were also recorded on each visit. These technologies allow quantifying oxygen saturation, hemoglobin content, and temperature as proxies of neo-vascularization. Ten patients from each arm underwent tissue biopsies at baseline, 2, and 4 weeks of treatment.
Results:
50 patients, 25 per treatment arm, are included in this analysis. The median time for achieving full closure in the collagen group was 17 vs. 9 weeks (reduction of 61.5% in the PLA group, p< 0.001). 32% vs 84% of wounds healed by 12 weeks in the collagen and PLA groups, respectively (p< 0.001). Spectral data showed significantly higher oxygen saturation and temperature in the peri-wound area and wound bed of the PLA-treated wounds after the second week of treatment. These features were even more evident in the oxyhemoglobin image maps. Molecular data showed that from baseline to 2 weeks of treatment, PLA had significant COL4A3 and CXCL5 upregulation. COL4A3 corresponds to Collage Type IV alpha 3, a major structural component of endothelial basement membranes, and CXCL5 or Chemokine (C-X-C motif) ligand 5 promotes angiogenesis and remodelling of connective tissues. From baseline to week 4, six genes were significantly upregulated: CSF2 (Colony stimulating factor 2), CXCL5 (Chemokine ligand 5), F3 (coagulation factor III), HBEGF (Heparin-binding EGF-like growth factor), IL1B (Interleukin 10), and TGFA (Transforming growth factor, alpha). Finally, from week 2 to week 4, ITGA3 and CSF2 were significantly upregulated. ITGA3 encodes cell adhesion molecules for endothelial and epithelial integrity. It also regulates tissue inflammation and controls granulocytes' and macrophages' differentiation. CSF2 is a granulocyte-macrophage colony-stimulating factor that helps restore the immune balance and stimulate the wound healing cascade. Histology data confirmed increases in CD31+ vessels and changes in CD68+ cells.
Discussion:
PLA matrices promote healing through direct effects on the angiogenesis and immune regulation of DFUs.

.jpeg)
