Case Series/Study
(CS-046) The Use of an Autologous Multilayered Leukocyte, Platelet and Fibrin Patch for Diabetic Ulcers: Does It Make a Difference?
Diabetes continues to have a devastating effect in the United States. 33% of diabetic foot ulcers(DFU) do not heal in a reasonable fashion and ultimately become “chronic” wounds. Approximately 20% of moderate to severe ulcers lead to some form of amputation, and patients with diabetes are up to 25 times more likely to lose their leg than those without. In a busy metropolitan wound center, many products to treat DFU are considered and used with varying degrees of success. Therefore, providers decided to trial the product to see if a difference was noted in wound healing. The results were pleasantly unexpected.
Methods:
24 DFU patients were trialed, having failed at least 10 applications of cellular tissue products and/or grafting. Of the 24, 11 closed(45.8%). No amputations or infections were noted which was extremely surprising.
Results:
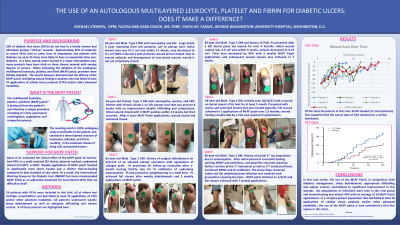
Of the 11 healed, three demonstrated exceptional healing with the use of this MLPF patch. One patient, a 44-year-old male with diabetic neuropathy and HIV, had a large Wagner Grade 3 extending from left posterior calf to plantar heel. Starting measurements were 14.0 cm x 4.8 cm; within 13 weeks, measurements decreased to 3.5 x 2.6 cm with posterior calf almost completely closed. After 8 more weeks, plantar heel measured 2.3 x 1.9 cm and continued improvement is noted. A 3rd patient, a 56-year-old female with diabetic neuropathy, anemia and CKD, presented with a Wagner grade 1 on her left plantar foot that had been present 8 weeks with no improvement. She was properly offloading and having compression applied as needed. The initial wound healed with 3C patch in 12 weeks but then recurred. Measurements at start of 2nd series were 1.0 x 1.4 x 0.1 cm and with 6 applications, wound healed. The final patient presented here was an 89-year-old male with a history of PAD and diabetes. The wound had been present for 4 months and several advanced therapies were tried. Initial measurement was 1.3 x 1.7 x 2.2 cm and within 6 weeks, wound measured 0.5 x 0.5 cm x 0.0 cm and went onto full closure.
Discussion:
In this case series, the use of the autologous patch, in conjunction with diabetes management, local sharp debridement and appropriate offloading, contributed to significant improvement in the wounds. The providers and program director deemed the trial a success and was able to bring in the patch to their wound center on a permanent basis.

.jpeg)