Case Series/Study
(CS-116) Use of fish skin xenograft in a patient with bullous pemphigoid
Bullous pemphigoid (BP) is the most common autoimmune subepidermal bullous disease. Topical or systemic corticosteroids are often used as the first-line treatment. However, long-term corticosteroid use may lead to significant side effects. Therefore, various adjuvant immunosuppressant therapies are used as steroid-sparing agents, with accumulating reports of biological treatments for severely recalcitrant BP1. The 1-year mortality rate of BP was 23.5%2. Superinfection caused by skin lesion ulceration is one of the important causes of disease death. Therefore, it is challenging to control infection and improve skin wound healing. Hence, advanced biological tissue, including a fish skin graft, are often used. This case report aimed to determine the clinical efficacy of Kerecis fish skin graft in BP complex wounds with exposed tendons and fascia.
Methods:
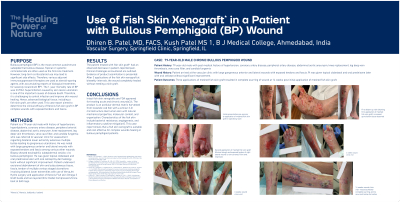
Patient is a 79-year-old male with history of hypertension, hyperlipidemia, coronary artery disease, peripheral arterial disease, abdominal aortic aneurysm, knee replacement, leg deep vein thrombosis, vena cava filter, and candida fungemia who was referred to vascular clinic for assessment regarding bilateral lower extremity extensive multiple bullae leading to gangrenous ulcerations. He was noted with large gangrenous anterior and lateral wounds with exposed tendons and fascia among various other wounds. Biopsy showed eosinophilic subepidermal vesicle, c/w bullous pemphigoid. He was given topical clobetasol and oral prednisone later with oral cellcept by dermatology team without significant improvement. Patient underwent excisional debridement of skin and subcutaneous tissue, fascia, tendon of multiple various staged ulcerations involving bilateral lower extremities with use of VersaJet Hydro surgery and application of Kerecis Fish skin Omega 3 Graft Guide and two layered (Zinc Oxide) Compression/Unna boot at both legs.
Results:
After 3 applications of the fish skin xenograft at biweekly intervals, the wound completely healed without needing a skin graft.
Discussion:
Omega 3 fish skin xenografts are FDA approved for treating acute and chronic wounds3,4. The product is an acellular dermal matrix harvested from Icelandic cod fish with a similar 3-D microstructure like human skin with natural mechanical properties, molecular content, and organization. Characteristics of the fish skin include bacterial resistance, angiogenesis, and inflammatory cytokine mitigation5. This case report shows that a fish skin xenograft is suitable and cost effective for complex wounds healing in bullous pemphigoid patients.

.jpeg)