Case Series/Study
(CS-089) Use of Negative Pressure Wound Therapy With Instillation in Non-Healing, Lower Extremity Wounds
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
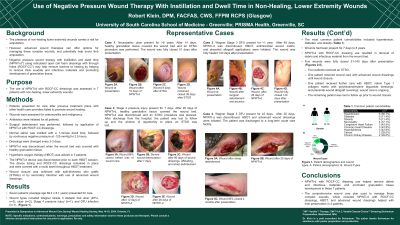
Introduction: Non-healing lower extremity wounds carry a risk for amputation. However, advanced wound therapies offer options for wound management, and potentially help avoid limb amputation. Negative pressure wound therapy with instillation and dwell time (NPWTi-d*) with reticulated open cell foam dressings with through holes (ROCF-CC†) use may help foster healing by providing hydromechanical removal of infectious materials, devitalized tissue, and wound debris along with promoting granulation tissue development. NPWTi-d with ROCF-CC dressing use was assessed in 7 patients with non-healing, lower extremity wounds.
Methods: Wounds were assessed for osteomyelitis and malignancy. Antibiotics were initiated for all patients. Surgical debridement was performed followed by application of NPWTi-d with ROCF-CC. Normal saline was instilled with a 1-minute dwell time, followed by negative pressure at -125 mmHg for 2.5 hours. Dressings were changed every 2-3 days. Once healthy granulation tissue covered the wound bed, NPWTi-d was discontinued. Hyperbaric oxygen therapy (HBOT) was utilized in 3 patients. The NPWTi-d device was disconnected prior to each HBOT session. The device tubing and ROCF-CC dressings remained in place and were covered with a moist towel throughout HBOT treatment. Wound closure was achieved with split-thickness skin grafts (STSGs) or by secondary intention with use of advanced wound dressings.
Results: Seven patients (average age 69.4 years) presented for care. Wound types included ulcer (n=2), Wagner Grade 3 diabetic foot ulcer (n=2), stage 4 pressure injury (n=1), open surgical wound (n=1), and amputation wound (n=1). NPWTi-d with ROCF-CC use resulted in granulation tissue development and hydromechanical removal of debris, devitalized tissue, and infectious materials. Four patients received STSGs after NPWTi-d use. One patient underwent further care with native Type I collagen matrix with polyhexamethylene biguanide dressings and placental wound allograft coverings. The remaining patient received advanced wound dressings until wound closure. All wounds were fully closed 51-140 days after presentation.
Discussion: NPWTi-d with ROCF-CC dressing use helped promote granulation tissue development and provided hydromechanical removal of infectious materials, devitalized tissue, and wound debris, in these 7 patients. The comprehensive wound care plan of NPWTi-d with ROCF-CC dressings, HBOT, and advanced wound dressings helped with limb preservation in 3 patients.
Methods: Wounds were assessed for osteomyelitis and malignancy. Antibiotics were initiated for all patients. Surgical debridement was performed followed by application of NPWTi-d with ROCF-CC. Normal saline was instilled with a 1-minute dwell time, followed by negative pressure at -125 mmHg for 2.5 hours. Dressings were changed every 2-3 days. Once healthy granulation tissue covered the wound bed, NPWTi-d was discontinued. Hyperbaric oxygen therapy (HBOT) was utilized in 3 patients. The NPWTi-d device was disconnected prior to each HBOT session. The device tubing and ROCF-CC dressings remained in place and were covered with a moist towel throughout HBOT treatment. Wound closure was achieved with split-thickness skin grafts (STSGs) or by secondary intention with use of advanced wound dressings.
Results: Seven patients (average age 69.4 years) presented for care. Wound types included ulcer (n=2), Wagner Grade 3 diabetic foot ulcer (n=2), stage 4 pressure injury (n=1), open surgical wound (n=1), and amputation wound (n=1). NPWTi-d with ROCF-CC use resulted in granulation tissue development and hydromechanical removal of debris, devitalized tissue, and infectious materials. Four patients received STSGs after NPWTi-d use. One patient underwent further care with native Type I collagen matrix with polyhexamethylene biguanide dressings and placental wound allograft coverings. The remaining patient received advanced wound dressings until wound closure. All wounds were fully closed 51-140 days after presentation.
Discussion: NPWTi-d with ROCF-CC dressing use helped promote granulation tissue development and provided hydromechanical removal of infectious materials, devitalized tissue, and wound debris, in these 7 patients. The comprehensive wound care plan of NPWTi-d with ROCF-CC dressings, HBOT, and advanced wound dressings helped with limb preservation in 3 patients.

.jpeg)
