Case Series/Study
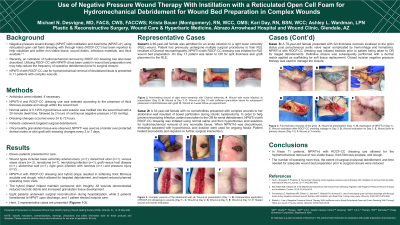
(CS-052) Use of Negative Pressure Wound Therapy With Instillation with a Reticulated Open Cell Foam for Hydromechanical Debridement for Wound Bed Preparation in Complex Wounds
Methods:
Antibiotics were initiated, if necessary. NPWTi-d and ROCF-CCC dressing use was selected according to the presence of thick fibrinous exudate and slough within the wound bed. Normal saline or 0.125% hypochlorous acid solution was instilled into the wound bed with a 20-minute dwell time, followed by 2 hours of continuous negative pressure (-125 mmHg). Dressing changes occurred every 24 to 72 hours. Patients underwent targeted surgical debridement. Once healthy granulation tissue was observed, NPWT‡ was used as a bolster over protected dermal matrix or skin graft with dressing changes every 3 to 7 days.
Results:
Eleven patients presented for care. Wound types included lower extremity arterial ulcers, (n=1), dorsal foot ulcer (n=1), venous stasis ulcers (n= 2), hematoma (n=1), necrotizing infection (n=1), graft vs host disease (n=1), abdominal wall (n=1), right groin infection with necrosis (n=1) and pressure injury (n=2). NPWTi-d with ROCF-CCC dressing and hybrid drape resulted in softening thick fibrinous exudate and slough, which allowed for targeted debridement, and helped reduced planned operating room visits. The hybrid drape§ helped maintain periwound skin integrity. All wounds demonstrated reduced necrotic debris and increased granulation tissue development. Eight patients underwent surgical reconstruction during hospitalization, while 2 patients transitioned to NPWT upon discharge. One patient elected hospice care.
Discussion: In these 11 patients, NPWTi-d with ROCF-CCC dressing use allowed for the hydromechanical removal of non-viable tissue, thick fibrinous exudate, and slough. The number of operating room trips, the extent of surgical excisional debridement, and time needed for adequate wound bed preparation prior to surgical closure were reduced.

.jpeg)
