Case Series/Study
(CS-020) Patient with Longstanding Pyoderma Gangrenosum ‘Got His Life Back’ in Just One Month
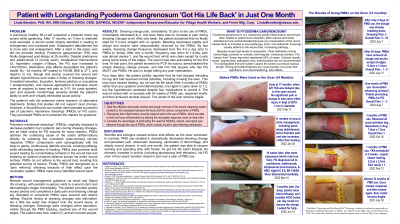
A previously healthy 65-yr-old presented with ~3-yr-old posterior lower leg wound sustained while gardening. Debridement at 17 months led to enlargement and increased pain, as did subsequent debridement. Pyoderma gangrenosum (PG) was diagnosed post-biopsy at 29 months. Pain, size, slough, and episodic hemorrhage increased despite prednisone and adalimumab (3 rounds each), intralesional triamcinolone x2, hyperbaric oxygen x10days, consistent elevation, and hypochlorous acid soaks 4-5/day at dressing changes.
By ~34 months, BP and BMI soared to 150/98 and 37.7, and HgbA1c increased to 9.9. Work and social activity were severely limited by pain and bleeding. Patient’s wife found a WoundSource.com poster demonstrating successful use of inflammation-controlling, continuously-debriding, moisture-balancing, pain-relieving dressing on PG ulcers (polymeric membrane dressings, PMDs). They purchased PMDs and contacted the makers for guidance in managing now ~140x120mm ulcer. Pain 3-10; 10 with dressing changes, standing, or walking, despite lidocaine ointment, ibuprofen, and various opioids.
Methods:
Remote wound management guidance, with periodic in-person visits to wound clinic and dermatologist, began immediately. Patient provided daily pain and dressing change log, and weekly wound photos. Standard or extra-thick PMDs were secured with stretch netting. Eliminated routine rinsing; water was added at dressing changes if wound bed was dry.
Results:
Sleep improved immediately. By day two, dressing change pain dropped from 10 to 2. Rest pain decreased to 0 at day 4, but activity pain spiked to 10 periodically for the first month. By one month, resumed work full-time with no bleeding, despite leg being dependent. Pain usually limited to 1 (neuropathic only). The patient had his life back! Ulcer closed after ~55 weeks of PMD use. HgbA1c gradually dropped to 7.2, but hypertension persisted despite four medications to control it.
Discussion:
Steroids and biologics caused serious side effects as the ulcer worsened. In contrast, PMD use led to atraumatic cleansing, dramatically decreased pain, hemorrhage elimination, and wound closure. In only one month, the patient was able to resume working and spending time with family (he got his life back). Despite this dramatic increase in activity (including limb dependency), this PG ulcer of four years’ duration closed in just over a year of PMD use.

.jpeg)