Case Series/Study
(CS-094) When Conservative Treatments Fail, What Next? The Use of an Autologous Multilayered Leukocyte, Platelet and Fibrin Patch for Diabetic Foot Ulcers
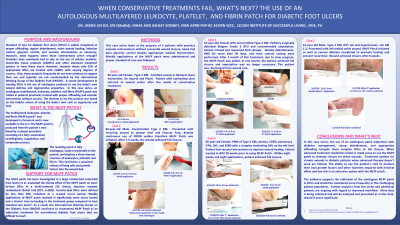
Standard of care for diabetic foot ulcers(DFU) is widely recognized as offloading, debridement, moist wound healing, glycemic control, and vascular intervention. However, what happens when these fail? Providers have commonly had to rely on the use of cellular tissue products(CTP) to treat these ulcers. However, research shows only 23% of appropriate DFU are treated with CTP with varying degrees of success. Also, these CTP frequently do not have evidence to support their use. A recent development in treating DFU is the use of autologous products. In this case series, an autologous, multilayered leukocyte, platelet, and fibrin patch(MLPF) was trialed in patients previously treated with proper offloading and vascular intervention.
Methods:
Seven patients will be presented in this case series. More patients initially received the patch but ended up falling out of the trial due to non-compliance, hospitalization, or lack of follow-up. Of the seven in this case series, all received the MLPF patch. The patient ages ranged from 54 to 93 years old. All had vascular interventions in the past. Some had poor control of their blood sugars despite appropriate medical interventions.
Results:
One patient, a 93-year-old female with diabetes and calcified vessels in bilateral lower extremities, presented after unsuccessful healing with 5 weeks of conservative treatment. After just four applications of the patch, the wound decreased in size from 5.5x3.4 cm to 1.1x0.9 cm. A second patient, a 54-year-old female, with uncontrolled diabetes at risk of limb loss, presented with a Wagner Grade 3 DFU and was being treated with a total contact cast. Again, in just four applications, this wound decreased substantially from 5.0x5.0 cm to 1.2 x 0.6 cm and achieved closure in five weeks. One other patient, a 66-year-old female, had been under the care of this wound clinic for 30 weeks prior to the use of the patch. She underwent complex vascular intervention to improved blood flow to the wound. After seven applications of the patch, the wound decreased 76% in volume and within eight weeks and eight applications, achieved full closure of the wound.
Discussion:
In this case series, the use of an autologous patch, in conjunction with diabetes management, sharp debridement and appropriate offloading, brought these complex diabetic foot ulcers to full closure when other interventions had failed. This supports the utilization of the autologous MLPF patch in DFU and should be considered more frequently in this challenging patient population.

.jpeg)