Clinical Research
(CR-018) A Service Evaluation Demonstrating the Protocolization of a Single-Use Negative Pressure Wound Therapy Device for Reducing Surgical Site Complication Risk following Gynecology and Gynecological Oncological Surgery
Surgical site complications (SSCs) pose many challenges for patients undergoing gynecology and gynecological oncological surgical procedures1-5.
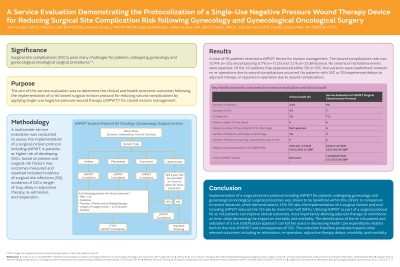
The aim of this service evaluation was to determine the clinical and health economic outcomes following the implementation of a risk based surgical incision protocol for reducing wound complications by applying single-use negative pressure wound therapy (sNPWT) for closed incision management.
Methods:
A multicenter service evaluation was conducted to assess the implementation of a surgical incision protocol including sNPWT, in patients at higher risk of developing SSCs, based on patient and surgical risk factors. Key outcomes measured and reported included incidence of surgical site infections (SSI), incidence of SSCs, length of stay, delay in adjunctive therapy, re-admission, and reoperation.
Results:
A total of 96 patients received a sNPWT device for incision management. The wound complications rate was 10.4% (n=10); encompassing 6.7% (n=7) SSI and 3.1% (n=3) dehiscence. No seroma or hematoma events were reported. Of the 10 patients that experienced either SSI or SSC, four patients were readmitted, however no re-operations due to wound complications occurred. No patients with SSC or SSI experienced delays to adjuvant therapy or required re-operation due to wound complications.
Discussion:
Implementation of a surgical incision protocol including sNPWT for patient’s undergoing gynecology and gynecological oncological surgical procedures was shown to be beneficial within this cohort. In comparison to recent literature, which demonstrated a 16% SSI rate, the implementation of a surgical incision protocol including sNPWT reduced the SSI rate by more than half (58%). This reduction therefore positively impacts other relevant outcomes, including re-admissions, re-operation, adjunctive therapy delays, morbidity, and mortality.

.jpeg)