Case Series/Study
(CS-104) Management of Enteroatomospheric Fistula with Negative Pressure Wound Therapy (NPWT)
Thursday, May 16, 2024
7:30 PM - 8:30 PM East Coast USA Time
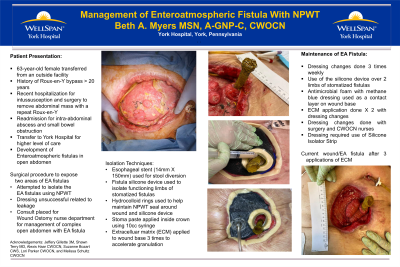
Introduction: 63-year-old Caucasian female admitted to the hospital with diagnosed intussusception of the small bowel. The patient had a history of a Roux-en-Y gastric bypass over 20 years prior. Surgery was required to correct the bowel defect and Roux-en-Y bypass was repeated. Over the course of several weeks the patient experienced a surgical incisional dehiscence and developed an enteroatomospheric fistula (EAF) in an open wound.
Methods: The Certified Wound Ostomy Continence Nurse (CWOCN) was consulted by the surgical team for management of the EAF as containment was difficult. Over the course of the patient's hospitalization several new/novel approaches were taken for wound dressing and containment of the effluent from multiple EAF in the open abdominal wound.
NPWT was used for wound dressing with the EAF contained suing a silicone device to divert effluent from the wound base. This became difficult related to the expanding size of the fistulas.
The surgical team developed a method to diver the effluent through the proximal limb of the fistula by using an Esophageal stent. The stent was placed endoscopically with the device extruding through the EAF. This allowed diversion from the wound base for several weeks and use of Extracellular Matrix (ECM) dressing. Three applications of ECM were provided to the wound base accelerating the formation of granulation tissue.
Results: The abdominal wound was shown to improve with the use of diversional techniques and the use of ECM. Wound dimensions continued to improve over the course of the 85-day hospital admission despite losing containment numerous times. The resulting wound base with 100% granulation tissue and half the original size by the time of transfer to an outside tertiary facility with a bowel program.
Discussion: This poster presentation reviews several new, novel approaches to the management of an EAF. The positive response of the wound with NPWT, the esophageal stent for diversion, the use of a silicone device, and the application of ECM allowed the patient to improve and advance to a higher level of care with a bowel program for eventual corrective surgery.
Methods: The Certified Wound Ostomy Continence Nurse (CWOCN) was consulted by the surgical team for management of the EAF as containment was difficult. Over the course of the patient's hospitalization several new/novel approaches were taken for wound dressing and containment of the effluent from multiple EAF in the open abdominal wound.
NPWT was used for wound dressing with the EAF contained suing a silicone device to divert effluent from the wound base. This became difficult related to the expanding size of the fistulas.
The surgical team developed a method to diver the effluent through the proximal limb of the fistula by using an Esophageal stent. The stent was placed endoscopically with the device extruding through the EAF. This allowed diversion from the wound base for several weeks and use of Extracellular Matrix (ECM) dressing. Three applications of ECM were provided to the wound base accelerating the formation of granulation tissue.
Results: The abdominal wound was shown to improve with the use of diversional techniques and the use of ECM. Wound dimensions continued to improve over the course of the 85-day hospital admission despite losing containment numerous times. The resulting wound base with 100% granulation tissue and half the original size by the time of transfer to an outside tertiary facility with a bowel program.
Discussion: This poster presentation reviews several new, novel approaches to the management of an EAF. The positive response of the wound with NPWT, the esophageal stent for diversion, the use of a silicone device, and the application of ECM allowed the patient to improve and advance to a higher level of care with a bowel program for eventual corrective surgery.

.jpeg)